by Catherine Avery
A church organist is asked to stay at her bench during the entire service, despite chronic arthritis pain. The same church provides an interpreter for the deaf, and wheelchair ramps for the disabled. It also allows a pregnant organist to move about the church freely to ease her back.
A woman with chronic back, hip, and leg pain is publicly upbraided by a stranger for parking in a handicapped spot, even though she has handicapped plates on her car.
A male moviegoer, standing in the back of the theatre to ease his aching back, is asked insistently to take his seat by the usher.
A pain patient's parents tell her to quit acting like a baby. "Where's the blood running out?" her mother asks her.
An anesthesiologist is suspected of angling for a disability when colleagues hear he is suffering from chronic neck pain due to a whiplash injury.
What do these scenarios have in common? They are all vivid, real life examples of the stigma of chronic pain.
A woman with chronic back, hip, and leg pain is publicly upbraided by a stranger for parking in a handicapped spot, even though she has handicapped plates on her car.
A male moviegoer, standing in the back of the theatre to ease his aching back, is asked insistently to take his seat by the usher.
A pain patient's parents tell her to quit acting like a baby. "Where's the blood running out?" her mother asks her.
An anesthesiologist is suspected of angling for a disability when colleagues hear he is suffering from chronic neck pain due to a whiplash injury.
What do these scenarios have in common? They are all vivid, real life examples of the stigma of chronic pain.
Stigma: A Fact of Life for Those with Chronic Pain
"It's easy to be paranoid when you hurt like hell and you're at the mercy of the health care system," says Dr. Bernard Filner, a Rockville, Md., pain management physician and chronic pain sufferer. He sustained a whiplash injury in a car accident 10 years ago, and still experiences neck pain and headaches.
Stigma, as defined by The Random House Dictionary as "a blemish on one's record or reputation is a pervasive fact of life for people with chronic pain.
The most wide-spread misconception about chronic pain is that it results from a psychological disturbance. Other common misconceptions are that those with chronic pain should be able to tolerate pain better as time goes on, that they are using pain to obtain narcotics, and that they exaggerate their pain for secondary gains, that is, for sympathy or financial gain.
The impact of stigma on chronic pain sufferers is devastating. "Stigma is a magnifier of pain," says Roberto Anson, 41, of Silver Spring, Md. "It boils down to one word ? discrimination."
Chronic pain often presents sufferers with a real "catch 22" dilemma. If they talk about their pain, they risk being perceived and labeled as hypochondriacs, or even worse?fakers or malingerers. On the other hand, if they hide their pain, others don't believe the pain is significant. It is enough to tax the patience of the most stoic person.
Health care professionals who see pain patients every day agree emphatically that stigma makes an already bad situation worse. Dr. Paul Buongiorno, a Fairfax, Va., psychiatrist who serves as medical director for Northern Virginia's Fair Oaks Hospital's Pain Management Program, sees patients daily who suffer from guilt, demoralization, and depression due to the negative perceptions of others. "Others feel you should pull yourself up by your bootstraps," Buongiomo says. "I don't believe that, though. You can't just talk yourself out of it."
Dr. Richard Baither, a Fairfax, Va., psychologist who treats chronic pain patients, refers to the "Job" syndrome. "People remember Job's patience," Baither says. "They feel they must have sinned. They ask themselves, 'What did I do wrong for these bad things to happen?"'
Noreen Freedman, a nurse and the coordinator of the Pain Resource Center at Washington Adventist Hospital, in Takoma Park, Md., says that her patients report a real sense of frustration about the public's perception of chronic pain. "You look fine, you must feel wonderful," others say, according to Freedman. "Pain is something you wear on the inside, not on the outside, " she notes. Freedman observes that men tend to emphasize the way chronic pain affects their work, while women tend to focus on the way it affects their relationships.
Stigma can be manifested in various ways?by raised eyebrows at work, by friends asking "Shouldn't you be feeling better by now?", and even by family members looking the other way or minimizing the problem.
Societal biases are also apparent ?theatres, restaurants, and the workplace are all designed for pain?free people, despite the staggering statistics that as many as one in three Americans suffers from chronic pain.
In addition, even very recent articles in the pain management literature demonstrate that negative stereotypes are alive and well even among professionals. Consider the following:
Indeed, people with easily visible proof of pain such as swollen joints, wheelchairs, canes or neck braces, often report that this tangible evidence of pain offers them validation in the eyes of others. Pain sufferers emphasize that a major factor behind the stigma is the invisible nature of most chronic pain.
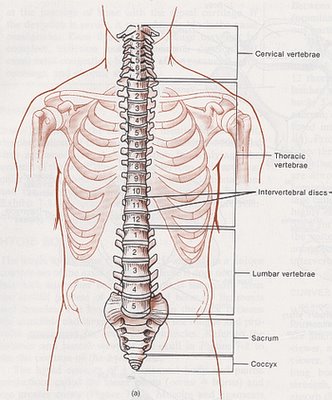
"You don't look like you're in pain," people tell Marty Heinrich, 39, of Damascus, MD. She asks them, "What does pain look like?" She has had chronic pain, originating with a broken back, since childhood.
Stigma, as defined by The Random House Dictionary as "a blemish on one's record or reputation is a pervasive fact of life for people with chronic pain.
The most wide-spread misconception about chronic pain is that it results from a psychological disturbance. Other common misconceptions are that those with chronic pain should be able to tolerate pain better as time goes on, that they are using pain to obtain narcotics, and that they exaggerate their pain for secondary gains, that is, for sympathy or financial gain.
The impact of stigma on chronic pain sufferers is devastating. "Stigma is a magnifier of pain," says Roberto Anson, 41, of Silver Spring, Md. "It boils down to one word ? discrimination."
Chronic pain often presents sufferers with a real "catch 22" dilemma. If they talk about their pain, they risk being perceived and labeled as hypochondriacs, or even worse?fakers or malingerers. On the other hand, if they hide their pain, others don't believe the pain is significant. It is enough to tax the patience of the most stoic person.
Health care professionals who see pain patients every day agree emphatically that stigma makes an already bad situation worse. Dr. Paul Buongiorno, a Fairfax, Va., psychiatrist who serves as medical director for Northern Virginia's Fair Oaks Hospital's Pain Management Program, sees patients daily who suffer from guilt, demoralization, and depression due to the negative perceptions of others. "Others feel you should pull yourself up by your bootstraps," Buongiomo says. "I don't believe that, though. You can't just talk yourself out of it."
Dr. Richard Baither, a Fairfax, Va., psychologist who treats chronic pain patients, refers to the "Job" syndrome. "People remember Job's patience," Baither says. "They feel they must have sinned. They ask themselves, 'What did I do wrong for these bad things to happen?"'
Noreen Freedman, a nurse and the coordinator of the Pain Resource Center at Washington Adventist Hospital, in Takoma Park, Md., says that her patients report a real sense of frustration about the public's perception of chronic pain. "You look fine, you must feel wonderful," others say, according to Freedman. "Pain is something you wear on the inside, not on the outside, " she notes. Freedman observes that men tend to emphasize the way chronic pain affects their work, while women tend to focus on the way it affects their relationships.
Stigma can be manifested in various ways?by raised eyebrows at work, by friends asking "Shouldn't you be feeling better by now?", and even by family members looking the other way or minimizing the problem.
Societal biases are also apparent ?theatres, restaurants, and the workplace are all designed for pain?free people, despite the staggering statistics that as many as one in three Americans suffers from chronic pain.
In addition, even very recent articles in the pain management literature demonstrate that negative stereotypes are alive and well even among professionals. Consider the following:
- A researcher who studied chronic back pain patients says his results support the theories of psychiatrist Thomas Szasz that chronic pain may become the "career" of patients who are "deeply committed" to the "sick role." The researcher concludes that medical treatment for such patients is ineffective since it "reinforces the pain patient role" (Gallon, 1989).
- Another researcher concludes that receiving disability payments for work?related injuries sets in motion a "stimulus?response/reward cycle" that is hard to break. Receiving workers' compensation payments, he believes, is likely to mean that the patient will always have chronic pain. The same researcher warns that "pathologic dependency," whether on one's family, physician, or drugs, is a "major obstacle to treatment" of chronic pain. He states that doctors who fail to recognize this "are destined to become entwined in the patient's dependency and become themselves an enabler of the patient's problem." (Newman, 1988).
- Still another article reported on a survey of physicians' attitudes toward chronic pain patients. While most of the 103 doctors surveyed as a group did not show evidence of negative bias toward chronic pain patients, there were key differences among different medical specialty groups. For example, anesthesiologists tended to believe that malingering is common among pain patients (Teaman and Cleeland, 1988).
- A psychologist who specializes in hypnosis argues that the management of chronic pain is actually the management of anxiety. He refers to the "seductiveness of demanding and receiving hell: from significant others" and "the mildly pleasant and/or euphoric effects of medication," which render pain "eventually necessary." He also cites examples of patients who use headaches to avoid sex, and playing with their children, and back pain to avoid mowing the lawn. The same pain management expert describes a helpful technique to unmask those pain patients who are receiving secondary gains from their pain. He asks four simple questions including, "Do you want to get better?" An angry response to this question indicates a poor prognosis while a simple, submissive "yes" indicates a good prognosis (Evans, 1989).
- Even recent medical research provides evidence of the stigma of chronic pain. The news media recently reported the development of a machine that determines whether patients are telling the truth about how much back pain they have by recording how patients move and how much force they exert in various directions. Insurance companies are reportedly showing great interest in this new device (The Wall Street Journal, September 26,1989.)
Indeed, people with easily visible proof of pain such as swollen joints, wheelchairs, canes or neck braces, often report that this tangible evidence of pain offers them validation in the eyes of others. Pain sufferers emphasize that a major factor behind the stigma is the invisible nature of most chronic pain.
"You don't look like you're in pain," people tell Marty Heinrich, 39, of Damascus, MD. She asks them, "What does pain look like?" She has had chronic pain, originating with a broken back, since childhood.
Where Does Stigma Come From?
Stigma arises from external sources such as health care professionals, family and friends, the public at large, government agencies and insurance companies, and even from other chronic pain sufferers. Stigma can also arise from within, with pain sufferers often experiencing guilt and blaming themselves for their pain.
Health care professionals often present formidable psychological obstacles to chronic pain patients. They want their treatments to produce results and when this doesn't happen, some blame the patient believing that the patient hasn't followed instructions properly, is receiving secondary gains from being in pain, or is simply imagining the pain.
Linda Lockaby, a Fort Meade, MD, musician has suffered from a variety of pain symptoms for the past five years, including rheumatoid arthritis, a nerve disorder in her shoulder, and myofascial pain. She reports that a rheumatologist diagnosed her as depressed, citing her weight loss and frequent bladder infections. He wasn't able to fit her symptoms with his diagnosis of arthritis so he advised her to "Just relax and see a psychiatrist."
Filner notes that patients tend to be sent from one doctor to another in search of relief. "It puts the burden on the patient," he says. Only once in several years of working with pain patients has Filner treated a true malingerer.
Even when doctors acknowledge that chronic pain is not rooted in psychological disturbance, Filner believes they may focus too much on helping patients accept their pain and not enough on finding ways to alleviate it. He wishes doctors would spend at least as much time ruling out additional treatment possibilities as they do in telling patients they just have to learn to live with the pain. "Many treatment options are available today," he says, "and more will be available tomorrow. I won't stop looking for causes and new treatment approaches." He terms his practice a "court of last resort."
Most pain patients report that family members especially spouses, feel a sense of frustration that they can't do more to alleviate the pain. Jill Gendleman, 39, of Bethesda, MD, has low back problems originating from scoliosis in childhood as well as almost daily headaches. Her husband of one year tries to help but feels frustrated that he can't make the pain go away.
Roberto Anson has an eight-year old daughter and has learned how difficult it is to be a parent who has chronic pain. "It's a challenge because I can't do some things," he says. Heinrich, who has two sons, ages 9 and 15, faces these same challenges. "I tell the boys I can't play ball, but I can play Monopoly," she says.
Heinrich finds that families often go to one extreme or the other -- either gushing all over the pain sufferer or acting angry and rejecting. As a child, she coped by hiding her pain, fearing that her family would reject her as defective and wouldn't love her if they knew the truth.
Lockaby says her mother refers to her chronic pain as "the little aches and pains of growing older," Lockaby is 34. Further, it has taken her some time to allow friendships back into her life. "People are afraid of us," Lockaby says, "because we look so normal. They're afraid they could be in the same position. They don't know how to act."
In the sixth grade, Gendleman was out of school for six months following back surgery. When she went back to school, her classmates avoided her. "It changed my life," she says now. "I became more of a loner. It was devastating." She attributes her classmates' behavior to their fear of "catching it".
Gendleman says a friend from her old job called her recently and commented, "God, I envy your life," referring to the fact that Gendleman has not -- because she cannot -- worked full time for the past two years. "Because many people can't relate to what life is like with chronic pain, my life just seems easier," she explains.
Freedman has seen evidence of job discrimination against workers with chronic pain. "The same problem again?" employers often ask pain patients. She notes that chronic pain cannot be objectively validated like heart disease or cancer, so therefore it can be more easily dismissed by employers.
This can be particularly problematic during job hunts. Freedman's patients report that potential employers tend to zero in on long periods when the person has been out of work, which they interpret as a warning flag. The applicant is then told there is someone "more qualified" for the job.
Anson, who has had chronic low back pain for the past two years as the result of a fall while roller skating, is a management analyst for the federal government. "People you work with daily forget about your situation," he says. "Sometimes, there are assignments that put your health at risk." Anson has a stand-up desk in his office which helps alleviate his pain.
Anson also note the flip side to the same coin. "Supervisors often make decisions based on their perceptions of what you can do," he says. They may decide that a person with chronic pain might not be up to a particular assignment without first checking that assumption with the individual.
In addition, Anson observes that someone with chronic pain can be seen as a source of distraction to others because they move around to increase comfort. "They think we have ants in our pants," he jokes. He often brings a cushion to meetings and arrives early to better adapt to the environment. In restaurants, he looks for a spot near the wall where he can stand up unobtrusively.
Filner was a practicing anesthesiologist 10 years ago when his car was hit from the rear while stopped at a red light. It was particularly ironic to have spent his professional life blocking pain in others and the be unable to stop his own pain. He discovered the when he wore a neck collar after his accident, others acted as if there really was something wrong with him. When the neck collar came off, he found out the hard way that no longer wearing tangible evidence of his pain changed the way he was perceived.
As Gendleman says, ours is a production?oriented society. She observes that people often think "If you can't produce, what good are you?"
"Insurance companies often want the person t prove that they've been injured on the job, say Baither. "They take an adversarial position?they're not interested in finding out what really happened. They string you out, and meanwhile you have no income and a bundle of medical bills. On top of that a lot of times they'll pressure you for a settlement.
The perception among many in the government and insurance companies is "Why would someone go back to work when they're better off not working?" However, patients only get paid a small portion of their salaries when they're disabled, Baither points out.
As Filner says, "You only get 30 to 50 percent of your salary on disability and you spend all your time in doctors' offices undergoing painful treatments. It totally affects your life. Why would anyone want I to that? It isn't something people want." In fact recent studies have shown that secondary gains are not a factor in the behavior of the vast majority of pain patients.
Filner feels the workers' compensation system and insurance plans seem to care more about saving money than getting people better. Insurance play also tend to promote surgery, believing it to be "quick fix." In reality, surgery not only exposes the person to the risks of a surgical procedure but often ends up being more expensive in the long run for everyone because it often makes the pain problems much worse.
Psychiatrist Buongiorno believes that the health care system has failed chronic pain patients. "Incentives in the system tend to make people with chronic pain worse, not better," he says. "The system is designed for acute care only and doesn't adequately address the needs of patients with ongoing health problems." This can be seen in insurance plans where surgery is covered but pain management programs are not.
Stigma against those with chronic pain can also lead to cancelled life and health insurance policies, not to mention insurance applications that are turned down. Lockaby had her life insurance cancelled due to her diagnosis of rheumatoid arthritis.
A recent article in the professional literature described the typical odyssey for an injured chronic pain patient, beginning with the trek from doctor to doctor and culminating without relief for the patient and only a meager legal settlement. Somewhere along the way, the patient gets labeled as a malingerer, which is underscored by the doctors who work for insurance companies. Finally, lawyers contribute to the problem by urging their clients to settle for small sums.
Filner points out that the "independent" medical exams required by insurance companies are anything but independent. Typically, the exams last about 15 minutes and arc conducted by doctors hired by the insurance company to evaluate patients. "It may be unethical because of conflict of interest," Filner says.
Filner believes that a truly independent examination would be aimed at arriving at a correct diagnosis and appropriate treatment plan, rather than at invalidating the patient's complaint of pain.
An unexpected and especially devastating source of stigma can be fellow pain patients. Same people fall into the trap of competing with others over who has more pain, Heinrich says. People sometimes view others who have reached the stage of acceptance of their pain as not being in much pain. On the other hand, those who have reached this stage sometimes look down an those still struggling with anger and grief.
A third reason for the stigma comes from the faulty reasoning that chronic pain must be due to character weakness or psychiatric illness. "Come on nothing can hurt that bad ?it must be in your head the thinking goes. Gendleman remembers a chiropractor advising her to see a psychiatrist after he observed that she was depressed. "Of course I was depressed. Who wouldn't be depressed sometime living with daily pain?"
"Doctors have treated me like a nut case," Heirrich agrees. "It's the most destructive thing." She firmly believes that, in most cases, pain leads to depression, not vice versa.
Filner points out that the accepted definition chronic pain stipulates having pain last for six months or more and not be amenable to medical treatment. This latter part of the definition ? not amenable to medical treatment ? assumes a psychological disturbance, Filner believes.
The stigma of chronic pain has other, more socio- logical roots in our culture. The attitudes we're taught as we grow up ? to keep a "stiff upper lip and not show you're emotions no matter how much pain and adversity we're faced with, are counter-productive.
Anson feels a particular stigma directed toward men. "In a mixed group, people turn to the men for muscle. One of the frustrations is that my pain is invisible. I walk in on my own; I look fine. They think 'What's the problem?"' Further, Anson notes, "Men are supposed to handle everything without shown their feelings. Men are not supposed to cry."
Ironically, recent much?publicized findings that positive imagery and visualization can improve health and reduce pain can inadvertently work against chronic pain sufferers and others with chronic medical problems. Sufferers themselves, as well as those around them, may wonder, erroneously, "If imagery is capable of reducing pain, doesn't that mean the pain is all in my head in the first place?" The logic behind these doubts is faulty since even terminal cancer pain can be eased by imagery and relaxation despite the fact that the pain is caused by the malignancy.
Health care professionals often present formidable psychological obstacles to chronic pain patients. They want their treatments to produce results and when this doesn't happen, some blame the patient believing that the patient hasn't followed instructions properly, is receiving secondary gains from being in pain, or is simply imagining the pain.
"You don't look like you're in pain people tell Marty Heinrich, 39, of Damascus,. Md. She asks them; "What does pain look like?" She: has had chronic pain, originating with a broken back, since childhood."Marty Heinrich visited her doctor after her second back surgery, still suffering from chronic back pain. "There's nothing wrong with this fusion," the doctor told her. "It's a beautiful fusion. You need a psychiatrist." She says that health care professionals have asked her, "Why are you hanging onto your pain?" or What's the payoff you're getting?"
Linda Lockaby, a Fort Meade, MD, musician has suffered from a variety of pain symptoms for the past five years, including rheumatoid arthritis, a nerve disorder in her shoulder, and myofascial pain. She reports that a rheumatologist diagnosed her as depressed, citing her weight loss and frequent bladder infections. He wasn't able to fit her symptoms with his diagnosis of arthritis so he advised her to "Just relax and see a psychiatrist."
Filner notes that patients tend to be sent from one doctor to another in search of relief. "It puts the burden on the patient," he says. Only once in several years of working with pain patients has Filner treated a true malingerer.
Even when doctors acknowledge that chronic pain is not rooted in psychological disturbance, Filner believes they may focus too much on helping patients accept their pain and not enough on finding ways to alleviate it. He wishes doctors would spend at least as much time ruling out additional treatment possibilities as they do in telling patients they just have to learn to live with the pain. "Many treatment options are available today," he says, "and more will be available tomorrow. I won't stop looking for causes and new treatment approaches." He terms his practice a "court of last resort."
Most pain patients report that family members especially spouses, feel a sense of frustration that they can't do more to alleviate the pain. Jill Gendleman, 39, of Bethesda, MD, has low back problems originating from scoliosis in childhood as well as almost daily headaches. Her husband of one year tries to help but feels frustrated that he can't make the pain go away.
Roberto Anson has an eight-year old daughter and has learned how difficult it is to be a parent who has chronic pain. "It's a challenge because I can't do some things," he says. Heinrich, who has two sons, ages 9 and 15, faces these same challenges. "I tell the boys I can't play ball, but I can play Monopoly," she says.
Heinrich finds that families often go to one extreme or the other -- either gushing all over the pain sufferer or acting angry and rejecting. As a child, she coped by hiding her pain, fearing that her family would reject her as defective and wouldn't love her if they knew the truth.
Lockaby says her mother refers to her chronic pain as "the little aches and pains of growing older," Lockaby is 34. Further, it has taken her some time to allow friendships back into her life. "People are afraid of us," Lockaby says, "because we look so normal. They're afraid they could be in the same position. They don't know how to act."
In the sixth grade, Gendleman was out of school for six months following back surgery. When she went back to school, her classmates avoided her. "It changed my life," she says now. "I became more of a loner. It was devastating." She attributes her classmates' behavior to their fear of "catching it".
Gendleman says a friend from her old job called her recently and commented, "God, I envy your life," referring to the fact that Gendleman has not -- because she cannot -- worked full time for the past two years. "Because many people can't relate to what life is like with chronic pain, my life just seems easier," she explains.
Freedman has seen evidence of job discrimination against workers with chronic pain. "The same problem again?" employers often ask pain patients. She notes that chronic pain cannot be objectively validated like heart disease or cancer, so therefore it can be more easily dismissed by employers.
This can be particularly problematic during job hunts. Freedman's patients report that potential employers tend to zero in on long periods when the person has been out of work, which they interpret as a warning flag. The applicant is then told there is someone "more qualified" for the job.
Anson, who has had chronic low back pain for the past two years as the result of a fall while roller skating, is a management analyst for the federal government. "People you work with daily forget about your situation," he says. "Sometimes, there are assignments that put your health at risk." Anson has a stand-up desk in his office which helps alleviate his pain.
Anson also note the flip side to the same coin. "Supervisors often make decisions based on their perceptions of what you can do," he says. They may decide that a person with chronic pain might not be up to a particular assignment without first checking that assumption with the individual.
In addition, Anson observes that someone with chronic pain can be seen as a source of distraction to others because they move around to increase comfort. "They think we have ants in our pants," he jokes. He often brings a cushion to meetings and arrives early to better adapt to the environment. In restaurants, he looks for a spot near the wall where he can stand up unobtrusively.
Filner was a practicing anesthesiologist 10 years ago when his car was hit from the rear while stopped at a red light. It was particularly ironic to have spent his professional life blocking pain in others and the be unable to stop his own pain. He discovered the when he wore a neck collar after his accident, others acted as if there really was something wrong with him. When the neck collar came off, he found out the hard way that no longer wearing tangible evidence of his pain changed the way he was perceived.
As Gendleman says, ours is a production?oriented society. She observes that people often think "If you can't produce, what good are you?"
Insurance companies often…take an adversarial position -- they're not interested in finding out what really, happened.Nowhere is that attitude more obvious or more potentially damaging as when government and insurance agencies use it against pain patients. Psychologist Baither pointed out that insurance companies have learned tactics for not paying chronic pain patients. For example, when a person is injured a work, the insurance company may question whether the injury is really work?related and request a hearing before the state workers' compensation commission. This hearing often doesn't take place until six or nine months later. In the meantime, a person who is unable to work isn't receiving a paycheck and maybe shouldering heavy medical bills.
"Insurance companies often want the person t prove that they've been injured on the job, say Baither. "They take an adversarial position?they're not interested in finding out what really happened. They string you out, and meanwhile you have no income and a bundle of medical bills. On top of that a lot of times they'll pressure you for a settlement.
The perception among many in the government and insurance companies is "Why would someone go back to work when they're better off not working?" However, patients only get paid a small portion of their salaries when they're disabled, Baither points out.
As Filner says, "You only get 30 to 50 percent of your salary on disability and you spend all your time in doctors' offices undergoing painful treatments. It totally affects your life. Why would anyone want I to that? It isn't something people want." In fact recent studies have shown that secondary gains are not a factor in the behavior of the vast majority of pain patients.
Filner feels the workers' compensation system and insurance plans seem to care more about saving money than getting people better. Insurance play also tend to promote surgery, believing it to be "quick fix." In reality, surgery not only exposes the person to the risks of a surgical procedure but often ends up being more expensive in the long run for everyone because it often makes the pain problems much worse.
Psychiatrist Buongiorno believes that the health care system has failed chronic pain patients. "Incentives in the system tend to make people with chronic pain worse, not better," he says. "The system is designed for acute care only and doesn't adequately address the needs of patients with ongoing health problems." This can be seen in insurance plans where surgery is covered but pain management programs are not.
Stigma against those with chronic pain can also lead to cancelled life and health insurance policies, not to mention insurance applications that are turned down. Lockaby had her life insurance cancelled due to her diagnosis of rheumatoid arthritis.
A recent article in the professional literature described the typical odyssey for an injured chronic pain patient, beginning with the trek from doctor to doctor and culminating without relief for the patient and only a meager legal settlement. Somewhere along the way, the patient gets labeled as a malingerer, which is underscored by the doctors who work for insurance companies. Finally, lawyers contribute to the problem by urging their clients to settle for small sums.
Filner points out that the "independent" medical exams required by insurance companies are anything but independent. Typically, the exams last about 15 minutes and arc conducted by doctors hired by the insurance company to evaluate patients. "It may be unethical because of conflict of interest," Filner says.
Filner believes that a truly independent examination would be aimed at arriving at a correct diagnosis and appropriate treatment plan, rather than at invalidating the patient's complaint of pain.
An unexpected and especially devastating source of stigma can be fellow pain patients. Same people fall into the trap of competing with others over who has more pain, Heinrich says. People sometimes view others who have reached the stage of acceptance of their pain as not being in much pain. On the other hand, those who have reached this stage sometimes look down an those still struggling with anger and grief.
The [health care] system is designed for acute care only and doesn't ade- quately address the needs of patients with ongoing health problems.Heinrich describes five stages that pain patients seem to experience: denial, anger, bargaining, grief, and acceptance. These same stages have been well documented as the ways in which people cope with loss and death. "You go through these stages when you lose your health,' Heinrich asserts.
A third reason for the stigma comes from the faulty reasoning that chronic pain must be due to character weakness or psychiatric illness. "Come on nothing can hurt that bad ?it must be in your head the thinking goes. Gendleman remembers a chiropractor advising her to see a psychiatrist after he observed that she was depressed. "Of course I was depressed. Who wouldn't be depressed sometime living with daily pain?"
"Doctors have treated me like a nut case," Heirrich agrees. "It's the most destructive thing." She firmly believes that, in most cases, pain leads to depression, not vice versa.
Filner points out that the accepted definition chronic pain stipulates having pain last for six months or more and not be amenable to medical treatment. This latter part of the definition ? not amenable to medical treatment ? assumes a psychological disturbance, Filner believes.
The stigma of chronic pain has other, more socio- logical roots in our culture. The attitudes we're taught as we grow up ? to keep a "stiff upper lip and not show you're emotions no matter how much pain and adversity we're faced with, are counter-productive.
Anson feels a particular stigma directed toward men. "In a mixed group, people turn to the men for muscle. One of the frustrations is that my pain is invisible. I walk in on my own; I look fine. They think 'What's the problem?"' Further, Anson notes, "Men are supposed to handle everything without shown their feelings. Men are not supposed to cry."
Ironically, recent much?publicized findings that positive imagery and visualization can improve health and reduce pain can inadvertently work against chronic pain sufferers and others with chronic medical problems. Sufferers themselves, as well as those around them, may wonder, erroneously, "If imagery is capable of reducing pain, doesn't that mean the pain is all in my head in the first place?" The logic behind these doubts is faulty since even terminal cancer pain can be eased by imagery and relaxation despite the fact that the pain is caused by the malignancy.
Some Good News
Fortunately, chronic pain has been gaining increasing public attention and media visibility in recent months. There is reason to be optimistic that the stigma of chronic pain will decrease as the public learns more about chronic pain and recognizes the vast numbers of sufferers in their midst.
The professional literature, too, is showing signs of change in the right direction. A nursing textbook on pain, for example, contains a thorough chapter on chronic pain which highlights and dispels common myths and misconceptions about pain patients [McCaffery and Beebe, 1989]. And more and more articles in the professional journals are addressing the issue of negative bias and stereotyping of chronic pain patients.
Pain patients are speaking out more publicly and getting more publicity. On the national level, they are fueling enormous growth in the membership of the Nation Chronic Pain Outreach Association. On a local level, they are banding together in support groups to fortify each other. It is only a matter of time until this expanding vitality impacts the public consciousness to squelch the stigma of chronic pain.
The professional literature, too, is showing signs of change in the right direction. A nursing textbook on pain, for example, contains a thorough chapter on chronic pain which highlights and dispels common myths and misconceptions about pain patients [McCaffery and Beebe, 1989]. And more and more articles in the professional journals are addressing the issue of negative bias and stereotyping of chronic pain patients.
Pain patients are speaking out more publicly and getting more publicity. On the national level, they are fueling enormous growth in the membership of the Nation Chronic Pain Outreach Association. On a local level, they are banding together in support groups to fortify each other. It is only a matter of time until this expanding vitality impacts the public consciousness to squelch the stigma of chronic pain.